There is a lot of confusion between these three terms. Many people do not know where they fit or if they even have any of these problems associated with glutens. Not everybody who has a gluten sensitivity will necessarily have digestive problems when consuming gluten but may have other health issues that are brought on by gluten. So how can this be if gluten comes in direct contact with the digestive tract? You may not know this, but your digestive tract has very few pain nerve endings and therefore you may be totally unaware of any problems until the inflammation and damage becomes uncontrolled or severe enough.
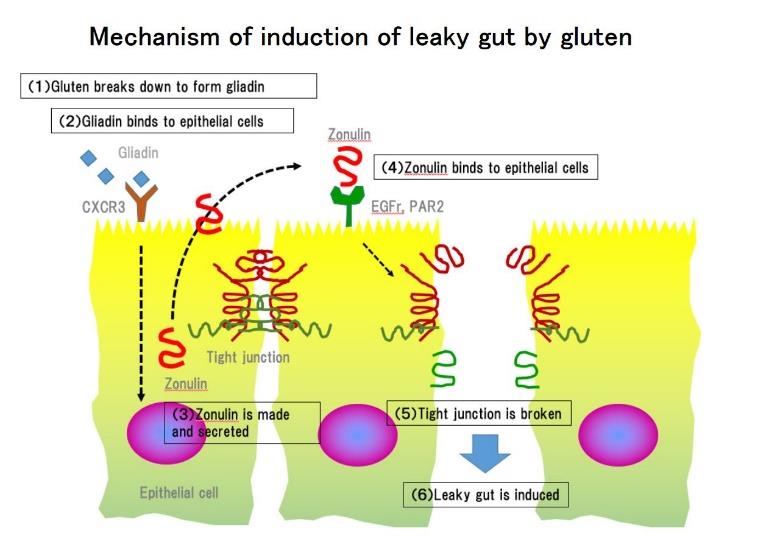
In our last newsletter, we pointed out that gluten can potentially be a major cause or contributor to inflammation in other parts of the body. Let us also remember that gluten can lead to malabsorption and damage to the intestines resulting in “leaky gut syndrome.” The bottom line is that the immune system response and type of genetic makeup determines a person’s reaction to gluten and which of these categories he or she falls into. We will explore these categories and how each one might affect a person’s health.
What is Gluten Sensitivity?
This is the broad all-encompassing term for any kind of immune response to gluten and under this umbrella we can include Celiac disease and wheat allergy. Gluten sensitivity is also known as non-celiac gluten sensitivity (NCGS). Some researchers estimate that 30-40% of people may have some level of gluten sensitivity.
Gluten sensitivity is determined by a group of genes found in DNA referred to as HDLQ. These genes influence the response of the immune system to gluten related proteins within certain grains. Recently, a test has been introduced that allows us to identify these specific genes. Using a simple mouth swab, it is possible to collect a sample of DNA to determine a person’s likelihood of gluten sensitivity and of any immune system response to gluten. The results provide evidence as to whether a person should avoid gluten, or not. This DNA test is available at our office.
The degree of your response to gluten is determined by the amount of gluten consumed, the types of gluten consumed, the status of your immune system, levels of antioxidants, levels of other nutrients, having proper upper digestive function, a balanced, diverse microbiome, and the degree of “leaky gut” or damage to the lining of your small intestines. The types of symptoms and health related issues tied in are numerous and some have been listed in our previous newsletter on gluten.
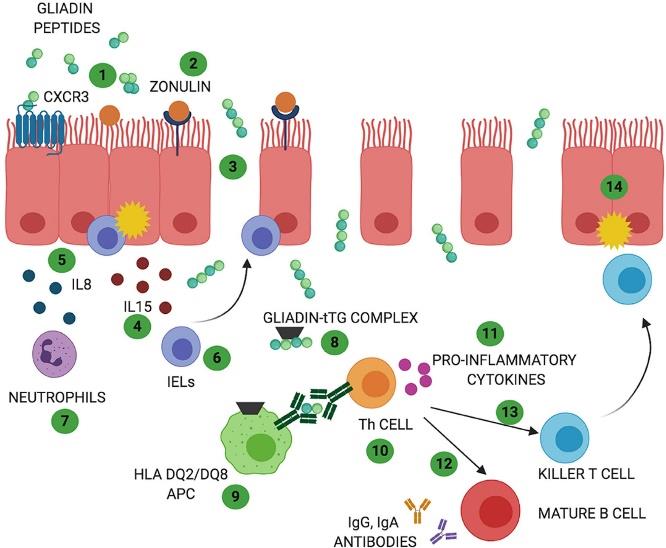
Gluten sensitivity or NCGS can cause inflammatory effects throughout the body. It also has a broad effect on the immune system and may not necessarily always cause the production of antibodies (immunoglobulins). It appears that it may affect major portions of the immune system referred to as the innate immune system. It may also stimulate other inflammatory pathways and lead to damage of the intestinal lining. The immune system is very extensive, complex, and about 70-80% is embedded in the intestinal tract. Therefore, the interaction of glutens with the intestines is critical. I have included a diagram of some of these interactions, below.
What is Celiac Disease?
Celiac disease is an auto-immune disease that is estimated to affect at least 1% of the population in the United States and worldwide. Many of these people go undiagnosed so the percentages could be even higher. On average, 33% of the population contains the genetic predisposition for Celiac disease. This type of gluten sensitivity has been studied the longest and is characterized by:
- Diarrhea and/or constipation
- Fatigue
- Bloating and gas
- Abdominal pain
- Nausea and vomiting
- Anemia
- Bone loss – osteopenia and/or osteoporosis
- Itchy, blistery skin rash known as dermatitis herpetiformis
- Mouth ulcers
- Headaches
- Numbness, tingling, balance problems and cognitive impairment
- Joint and muscle pain
- Multiple nutrient deficiencies
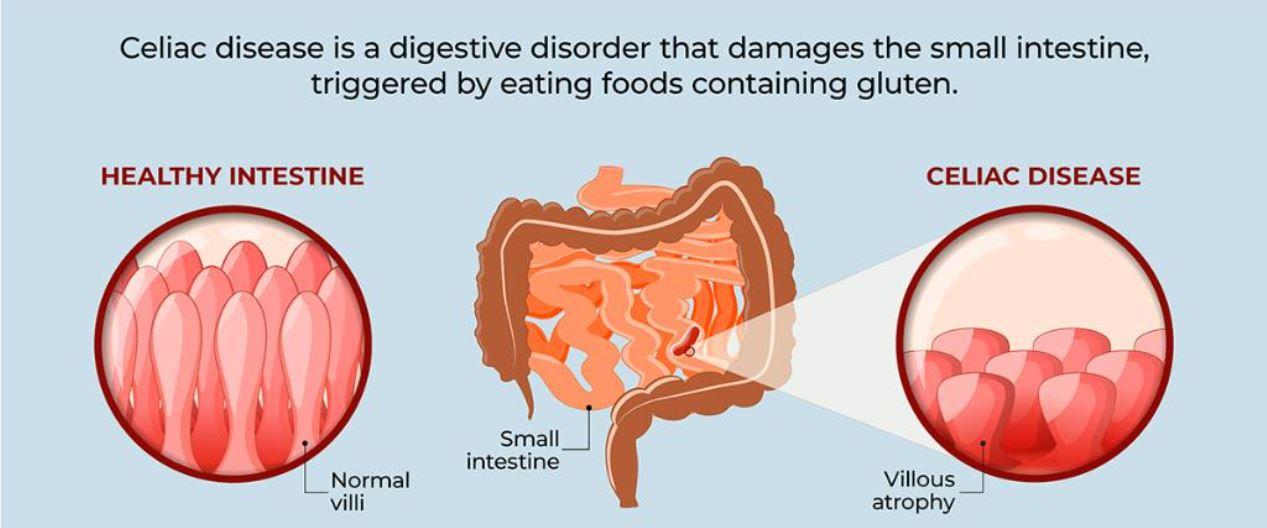
It is also, but not always, identified by visible damage to the lining of the small intestine called villous atrophy. This is where the finger like projections, of the small intestine, are damaged and flattened. As a result, the small intestine’s ability to absorb critical nutrients is compromised.
Often people with Celiac disease will have specific HLDQ genes called HLDQ2 and HLDQ8. Additionally, they are likely to have certain types of antibodies that form because of damage to the intestinal lining. These antibodies can be tested for using a “Celiac panel.” However, sometimes this panel may show negative due to a lack of sufficient intestinal damage, a generally “poor or weakened” immune response, or limiting antibodies testing to a singular protein component of gluten called alpha gliadin. Remember, there are many different proteins found in glutens of various grains. Therefore, if a person is not tested for these other components or grains, he or she may not fully identify the Celiac disease or gluten sensitivity. Thus, a comprehensive test is very important.
What is a Wheat Allergy?
A wheat allergy is considered a “true” allergy to the various proteins in wheat, and it is an extremely specific immune response. There are specific immune cells (B Lymphocytes) that are involved with this response to wheat gluten. They will activate other cells that produce specific antibodies called immunoglobulin E or known as IgE. They then attach to mast cells that release large amounts of histamine. This can result in classic allergy symptoms and if severe enough cause anaphylaxis. Usually those that have a wheat allergy get a rapid, within minutes, response to wheat. Such response may result in itching, swelling lips and tongue, trouble breathing, nausea, and abdominal pain.
Summary
Technically, the term gluten sensitivity could be used as an umbrella term that entails any type of immune system response to gluten and its other associated compounds. So, even though there are specific characteristics for celiac disease and wheat allergy, they can still come under the broad banner of gluten sensitivity.
Furthermore, 70-80% of the immune system is embedded within the digestive tract and is stimulated by gluten which then releases messenger compounds such as cytokines. Some of the “activated” cells that started in the intestines can spread throughout the body, as well. The combination of cytokines, activated cells, and antibody complexes can begin an inflammatory response throughout the body. Depending upon the organ or tissues that become inflamed a diagnosis can then be assigned. However, the real underlying cause of the inflammation, due to gluten, may go undetected and instead treated symptomatically.
Many times, the ultimate result of this gluten reaction results in, or contributes to, autoimmune disorders throughout the body. A disorder that is quite common is known as Hashimoto’s thyroiditis. Hashimoto’s is the most common cause of hypothyroid problems and it is suspected that 60-70% of all hypothyroid conditions are due to this autoimmune attack on the thyroid. We will discuss Hashimoto’s in a future newsletter and video!
Luckily, there are several things a person can do to prevent or repair some of the damage that has occurred due to glutens. This can be done by primarily avoiding different glutens and cleaning up the diet. He or she can also decrease the resultant inflammation and assist in restoration of damaged tissue/organs to provide valuable nutrients which balances the immune system/organs and helps to heal “leaky gut syndrome.” Additionally, we will explore this topic deeper in our next newsletter.
Last, if you have any questions relating to gluten health issues, please feel free to contact our office. If you are interested in the “gluten” DNA test, Celiac panel, or other testing, such as the “leaky gut test” as mentioned above, please call our office at (480) 732-0911 to schedule an appointment. My office staff is happy to assist you.

